As COVID-19 (Coronavirus) continues spreading across the globe, more individuals and institutions must decide how they’ll respond to the virus. Determining effective response protocols and practices is a complex task that falls to medical and public health professionals across the globe. However, communicating a selected response plan is often the responsibility of institutions such as businesses, schools, and public organizations that might not have experience conveying safety-critical information.
Effective medical and public health policies are the primary factors in controlling the virus’ spread and in treating those who are affected by it. However, ineffective communication of procedures and plans can undo even the best planned policies. If the intended audiences miss, misinterpret, or fail to comply with communications related to the virus, they are more likely to behave in ways that might facilitate the virus’ spread and interfere with its treatment.
As a father of school-age children, I’ve encountered various messages, posters, and signs that communicate schools’ policies for dealing with the ongoing COVID-19 outbreak. As a human factors engineer, I couldn’t help but notice the numerous design and communication shortcomings that limited the materials’ effectiveness.
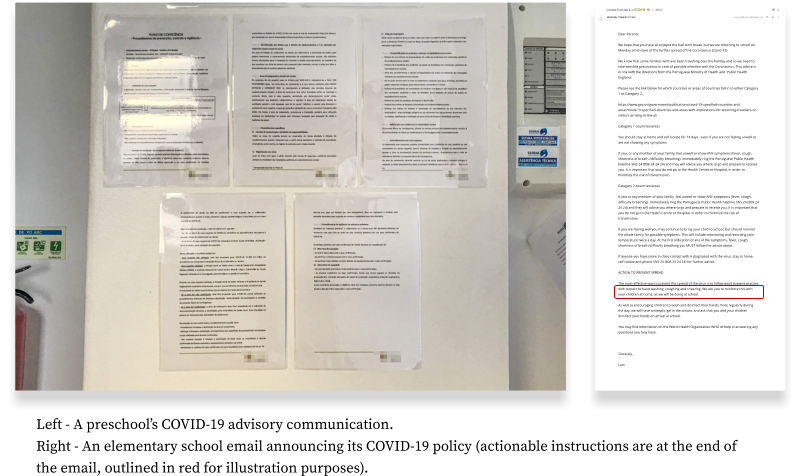
My daughter’s preschool hung a five-page COVID-19 policy full of small text and scientific references amid the monthly birthday announcements in the school’s hallway, where it is unlikely to be noticed or read. My son’s elementary school described its quarantine policy in a passively voiced sentence lost at the very end of a long email.
Unsurprisingly, parents in both schools have been confused by the communicated policies and failed to follow the provided guidance effectively.
Communicating safety-critical information requires a consideration of human factors — the behaviors, characteristics, and tendencies that affect how people respond to stimuli in products or informational materials. The discipline of human factors engineering, which is used to prevent use errors in safety-critical products such as airplanes and medical devices, can provide helpful guidance for communicating information related to the spread of infectious diseases.
If you’re in the process of defining, designing, or communicating COVID-19-related policies to your customers, employees, or your general community, here are three basic guidelines to help increase the likelihood that people will notice, understand, and follow your guidance.
Consider your audience
A key tenet of human factors engineering is “know your user” — develop an understanding of the physical, cognitive, and social characteristics that affect how people will use the information or product you are designing. Factors such as a person’s eyesight or literacy level have a direct and obvious effect on their ability to notice and understand information on an informational poster, for example.
However, some human characteristics change in response to certain contexts. Cognitive science research has shown for example that people under emotional duress are more likely to commit reading errors and are more likely to misinterpret information. If you consider your audience’s constant and context-specific characteristics, you’re more likely to craft communications that match their capabilities and expectations.
Suggestions
- Avoid making false assumptions about your audience’s knowledge level — Although COVID-19 has garnered a lot of attention, many people remain unaware of the virus’ rapid spread, its potential dangers, and the best practices for avoiding transmission. It’s better to state the obvious than to leave out key details that might be unknown to some.
- Make sure information is legible — People must be able to see and read information before they can use it. Make sure to use large, high contrast text to get people’s attention and to facilitate reading. This is especially critical if you’re trying to communicate with an older audience that is more likely to have vision impairments.
- Consider cultural differences that might affect your audience’s interpretation of information — The spread of COVID-19 is a global crisis that has already affected many countries. Different countries have responded in different ways and members of your audience might have different mental models of the current situation, which might affect how they interpret the information you’re providing.
Focus on key details
To ensure effective communication, the US military encourages its personnel to practice the “BLUF” principle. The acronym, which stands for Bottom Line Up Front, is a good guideline for sharing safety-critical health information as well. Making actionable information prominent increases the likelihood that your audience will notice it and comply with the instructions.
Given the large amount of disinformation and lack of certainty surrounding COVID-19, it is critical to communicate suggested behaviors and practices in an obvious and concise manner. Using visual formatting, such as large headers and color-coding, can also help draw your audience’s attention to key points you wish to communicate.
Suggestions
- Focus on actionable information — When communicating public health policies, emphasize the information intended to guide your audience’s behavior or practices. While added contextual information might be helpful, it should appear secondary to the primary guidelines you provide.
- Be concise — Busy people tend to skim information and ignore long texts. Stressed people struggle to focus on complex details. Keep your messages short and direct so that most of your audience will understand key takeaways.
- Use graphics where appropriate — Complement your textual communications with illustrations and icons that help draw attention to key points and help demonstrate encouraged behaviors.
- Provide explanations and cite your sources of information — Your audience will be more likely to follow guidance if you briefly explain the reasons for suggesting certain actions. Similarly, people are more likely to pay attention to guidance if it originates from a trustworthy source.
Use clear, direct, and accurate language
When communicating policies about viral outbreaks, there is an appropriate and understandable interest in avoiding the fear and panic that could result from an alarmist message. However, this interest can result in a tendency to soften the message by using vague language. Such a tendency will likely make the communication more difficult to understand and to follow for at least some of the audience.
This tendency can also lead to communications that focus more on “damage control” intended to calm the audience and maintain the messenger’s reputation than on disseminating practical information. While there is value in spreading reassuring messages, they should be secondary to details that will have a more practical effect on meeting the public health goals at hand.
Suggestions
- Use simple language — Many people have relatively low literacy skills and struggle to read texts that include sophisticated language (i.e., words with many syllables, uncommon terms, etc.). When communicating health-related information, some people tend to include scientific language that might be beyond the reach of the basic reader. Aim to use plain, practical language instead.
- Avoid passive voice — If a health-related communication is intended to spur a specific action, use active voice and imperative commands in your writing.
- Minimize the need for you audience to find additional information elsewhere — It is often appropriate to refer your audience to official guidance provided by governmental health organizations, such as the CDC and WHO. But, in many cases, it can be more effective to excerpt key content from these organizations’ guidance and include it directly in your communications, thereby minimizing the need for people to search for key information elsewhere.
The guidelines above provide a mere starting point for writing and designing effective guidance. When designing safety-critical communication, it is a good idea to also evaluate a design’s effectiveness by conducting usability tests or other evaluation techniques to ensure that people interpret your guidance as expected.
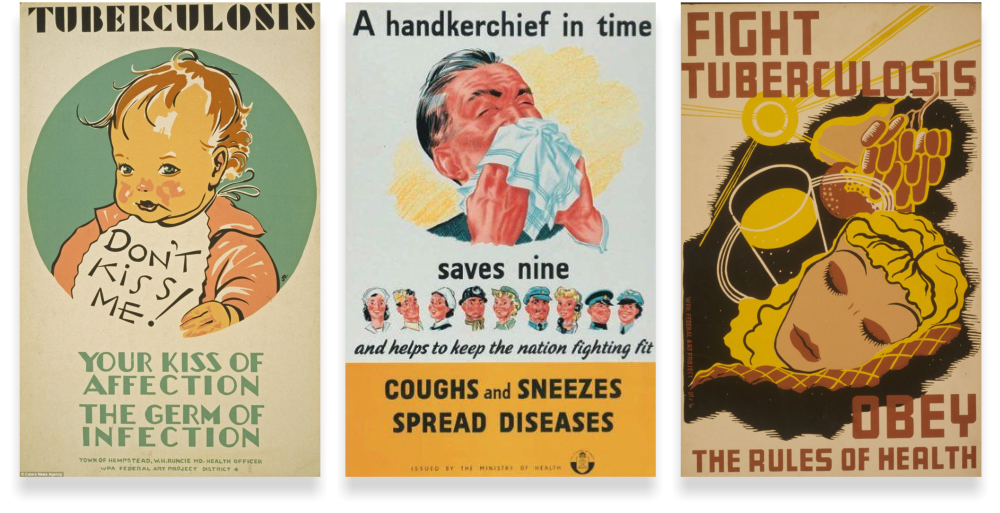
Finally, while COVID-19 is a novel virus, the practice of informing the public about health risks through visual communications has a long history. If you’re seeking inspiration for clever ways to communicate health information, consider exploring vintage health posters from the NIH’s library.